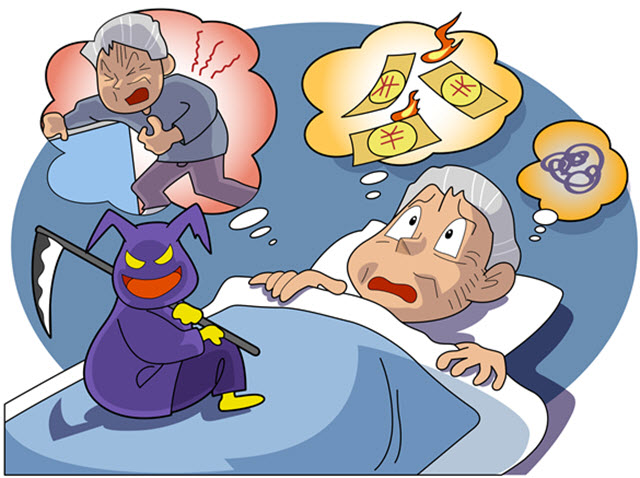
Insomnia and the Elderly
Chronic Sleep Disturbances in Older Adults Pose Challenges
Insomnia and general sleep disturbances are common among older adults and the elderly. But are pernicious in that they can lead to serious medical side effects with far-reaching ramifications.
Fact is, the incidences of insomnia typically increase as you grow older and often affect more women than men. Why is aging key? As you age you are more apt to experience physical, psychological, social, and situational changes and conditions that can wreak havoc with your sleep. These can become key causes for elderly insomnia and they include:
- Menopause
- Other hormonal changes
- Changes in brain activity
- Changes in natural sleep patterns
- Medication and ailments
- Social changes
- Anxiety
- Depression
The latter, depression, is deeply interconnected to insomnia. In many cases of chronic sleep deprivation depression may be a primary or a secondary factor and the elderly are commonly stricken. Elderly depression often goes untreated, is ignored, and is passed off as signs of aging. And studies have shown that 80% of those suffering depression also report regular symptoms of insomnia. *
The common insomnia pattern reported by older adults is late, terminal or advanced sleep-phase. This means you may fall asleep at night without disturbance, but wake up in the wee hours of the morning and are unable to return to sleep. This pattern is most consistent with chronic insomnia.
Diagnosing Insomnia in Older Adults
Doctors are already challenged diagnosing insomnia because the symptoms of insomnia are usually inspired by other root causes. So there are primary and secondary diagnoses and often you’re facing dual treatments. The process of diagnosis includes examination of medical history, past and present, a battery of sleep and behavior related questions that you must candidly answer and possibly further testing at a sleep study facility.
- Difficulty #1: many older adults avoid the doctor, thus passing off sleep disturbance as a natural part of their lives.
- Difficulty #2: unraveling the often confusing mix of medication effects, physical factors, and social factors that let a doctor read clues.
- Difficulty #3: treatment and long-term compliance.
Treatments for Elderly Insomnia
Prescription sleep aids, also called hypnotics, have long been a standard tool in the fight against sleep disturbance and insomnia. Hypnotics are still used widely, but among the elderly the use of benzodiazepine receptor agonist drugs carries risks. Benzo side effects include confusion, dizziness, and drowsiness which can lead to falls or other physical accidents. Auxiliary side effects like this can have far-reaching effects.
Doctors more frequently prescribe non-benzodiazepines. Popular brand names include Ambien, Lunesta and Sonata. But even these are only recommended for short-term treatment. Because elderly insomnia is often chronic, these medications are rarely a standalone solution.
In combination with or as an alternative to pharmacotherapy, cognitive behavioral therapy (CBT) is becoming widely accepted for its non-drug applications. Studies have shown that CBT can be a much more effective and permanent solution to chronic insomnia. CBT combines a medley of therapies—behavioral (sleep hygiene), psychological, physical—that treat the patterns of insomnia.
Common treatments for elderly insomnia include:
- Prescription sleep aids - non-benzos preferred
- OTC sleep aids
- Cognitive behavioral therapy
- Natural therapies—melatonin, valerian, other herbs
- Hypnosis
Insomnia Risks for the Elderly
Insomnia can become quickly chronic in an elderly person and when it does the lifestyle can be critically affected:
- Lack of concentration can lead to accidents like leaving the stove on, leaving doors unlocked
- Increased clumsiness can lead to physical falls and other accidents
- Constant tiredness can lead to auto accidents
- Avoidance of symptoms can lead to clinical depression, which heightens sleep disturbance.
